Scarring Alopecia
Scarring, or cicatricial alopecia, is an inflammatory condition that destroys hair follicles, causing scarring and permanent hair loss. The Mount Sinai’s Alopecia Center of Excellence can help. Dermatologists have deep experience diagnosing and treating this form of alopecia
Generally, cicatricial alopecia is caused by inflammation, which damages the hair follicle. Damage can also stem from a trauma such as a burn or serious infection. The inflammation can involve different types of cells, including lymphocytes, natural killer cells, or several cell types.
Cicatricial alopecia affects both men and women but is rare in children. Researchers do not yet fully understand the causes of the disease. But we believe that inflammation destroys the stem cells and oil glands of the hair follicle, leading to scarring (called fibrosis) and hair loss. It is not thought to be hereditary. The best way to prevent fibrosis and permanent hair loss is to intervene early.
Cicatricial alopecia progresses differently in different people. Hair loss may develop slowly over years with too few symptoms to notice. In some people, it progresses rapidly over months, causing burning and itching. The affected areas could turn red and develop scaling or pustules.
At the Center of Excellence, we offer skilled care for cicatricial alopecia, based on the newest research. Mount Sinai has performed much of the research into this disease. Diagnosing cicatricial alopecia involves a clinical exam and a biopsy, which involves taking and examining a small sample of affected tissue. The biopsy provides information about the type, location, and severity of inflammation.
Treatment depends on the type of cells that are causing the inflammation in your body. Options may include systemic (oral or biologic), topical, or injected anti-inflammatory medications. We uniquely offer new clinical trials for scarring alopecia.
Scarring alopecia can affect any healthy man or woman. It is not contagious and may not always have a genetic link up. Some types are seen more commonly in women than in men. Pseudopelade is a type of scarring alopecia that mainly affects adult women. Generally, Scarring alopecia is not seen in children; however, some specific type can affect adolescent men
Scarring alopecia is classified as primary, secondary and developmental/hereditary alopecia.
Primary scarring alopecia: This is caused as the hair follicle is irreversibly destroyed and replaced by fibrous tissue. In primary scarring alopecia the hair follicle is the main target of destruction from where the disease begins. The hair cannot be regrown because the stem cells in the bulge of hair root are totally destroyed. The hair follicle is mainly affected by inflammatory cells such as lymphocytes, neutrophils, or combination of these. Based on the type of inflammation causing cells primary scarring alopecia is further classified as lymphocytic, neutrophilic or mixed alopecia.
- Neutrophilic Cicatratial alopecia: Folliculitis decalvans and dissecting cellulitis of the scalp fall under this category. Both the conditions are seen predominately in adolescent males or young adults.
- Lymphocytic alopecia: Lichen planopilaris (lichen planus follicularis), chronic cutaneous lupus erythematosus, frontal fibrosing alopecia, acne keloidalis nuchae, central centrifugal cicatricial alopecia and Brocq pseudopelade are caused by lymphocytes.
Secondary scarring alopecia: This too is a type of irreversible scarring alopecia. However, the hair follicles are secondarily damaged as a result of inflammation or destructive process to the skin that eventually affects the hair follicles. This type of alopecia occurs when the follicle are destroyed due to burns, cancers, trauma or radiation therapy.
Developmental/hereditary alopecia: This is caused by one or more factors such as genetics, hormone imbalances or natural ageing process commonly known as Male / Female pattern baldness.
Lymphocytic alopecia such as Lichen planopilaris and frontal fibrosing alopecia are mainly treated using topical, intralesional and oral therapies. Application of topical corticosteroid creams helps to control the itching or burning in lesions on scalp. In some cases an injection of corticosteroid is given in the inflammatory lesion. This helps to stop hair loss at the site of injection. Injections may need to be repeated every 6 to 8 weeks. Prolonged use of steroids injectable as well as topical can cause the shrinking of skin at the site of use.
Oral medications given to treat lymphocytic oral medication include antimalarial drugs, oral corticosteroids, and oral retinoids.
Since some lymphocytic scarring alopecia are known to aggravate on exposure to sunlight use of sunscreen agent with good sun protection factor (SPF) is also recommended.
What are the side effects of treatment for Lymphocytic scarring alopecia?
- The antimalarial medications may cause side effects such as abdominal pain, anorexia, skin hyperpigmentation, hematologic changes and ophthalmologic damage. Therefore, regular monitoring for the development of retinopathy is needed in patients who are taking antimalarial treatment for 3 to 6 months.
- Repeated use of steroids may cause steroid-induced dermal atrophy
Treatment modalities for Lymphocytic scarring alopecia can be summarised as follows,
- Topics steroids applied on the lesion
- Injectable steroids
- Oral medications such as antimalarial drugs , corticosteroids, and retinoids
- Broad-spectrum sunscreen agents
Since Staphylococcus aureus is the main causative organism people with folliculitis decalvans are advised to use antiseptic shampoo. Topical creams containing benzoyl peroxide or clindamycin are recommended in mild cases. The severe cases often require treatment with oral antibiotics. Other type of neutrophilic scarring alopecia called dissecting cellulitis is usually treated with isotretinoin.
What are the side effects of treatment for neutrophilic scarring alopecia?
- Prolonged use of some antibiotics such as oral clindamycin may cause diarrhoea
Treatment modalities for Lymphocytic scarring alopecia can be summarised as follows,
- Topical creams containing benzoyl peroxide or clindamycin
- Antiseptic shampoos
- Oral antibiotics for severe lesions
- Oral retinoid such as isotretinoin
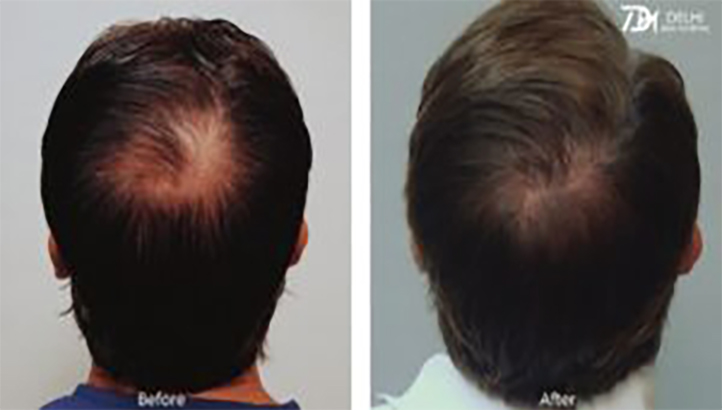
Surgical treatment for scarring alopecia is recommended in people who show lesions that are stable in size. The surgery can be performed only if the inflammation causing the hair loss is under control for at least one year. The suitable candidates can undergo a treatment called scalp reduction surgery, which can be complemented by hair transplantation, for best effects.
Hair care is very important once you know you are suffering from scarring alopecia. You can continue the use of your regular hair care products after consultation with trichologist. Here are some hair care tips for people with scarring alopecia
- Do not use any hair products including shampoos or other styling products that may have harsh chemicals and irritate the scalp
- Protect your hair and scalp with hat or scarf and also wear broad-spectrum sunscreen on a daily basis as some types of scarring alopecia worsen on exposure to UV light.
- Use antiseptic shampoos as recommended by your dermatologist to reduce the inflammatory lesions
- Continue the course of antibiotics as prescribed to you
- Use hair wigs or other hair pieces to camouflage the bald patches
Book Your Free Consultation Now
Other Treatment
-
Medical Treatment
Treatments prescribed by doctors can be classified using one or several of the following methods: Medical, surgical, or medico techniques
-
Non-surgical treatment
Non-surgical medical procedures are used to diagnose, measure, monitor or treat problems such as diseases or injuries that don’t require surgery
-
Laser therapy for hair growth
Low-level laser therapy — also referred to as red light therapy and cold laser therapy — irradiates photons into scalp tissues
Gallery